Polycystic Ovary Syndrome and Mental Health
Let’s talk about it!
Polycystic ovary syndrome (PCOS) is a common hormonal condition that affects both physical health and mental wellbeing. While it is often discussed in terms of reproductive or metabolic symptoms, many individuals with PCOS also experience anxiety, depression, and emotional distress alongside physical changes and symptoms.
In this post, I explore how PCOS can affect mental health, why these impacts can occur, and how therapeutic support can play a meaningful role in navigating the emotional experience of living with PCOS.
What is PCOS?
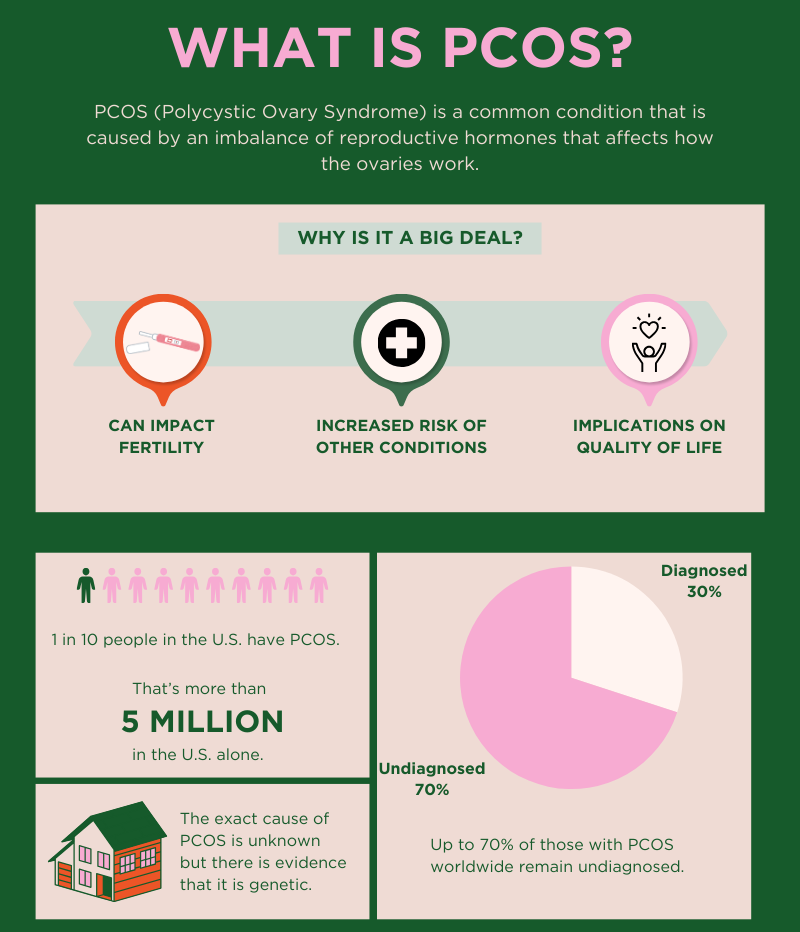
According to the World Health Organization, PCOS affects an estimated 8 to 13% of individuals born as females of reproductive age, and up to 70% of cases remain undiagnosed (World Health Organization, 2023). For many, this delay in diagnosis can feel confusing, frustrating, or even invalidating—especially when symptoms have been minimized or misunderstood.
Beyond its physical effects, PCOS can have a significant emotional and psychological impact. Changes related to weight, hormones, fertility, or appearance can affect self-esteem and our sense of identity. Social pressures—such as expectations around fertility or “what bodies should do”—can further intensify stress, shame, or grief. Over time, these experiences very likely contribute to anxiety, depression, and/or feelings of isolation.
For many individuals, having a space to process these experiences—rather than carrying them alone—can be an important part of care. Emotional support, including therapy, can help people navigate the mental health aspects of PCOS with more compassion, clarity, and self-understanding.
Overview of PCOS Symptoms and Comorbid Conditions
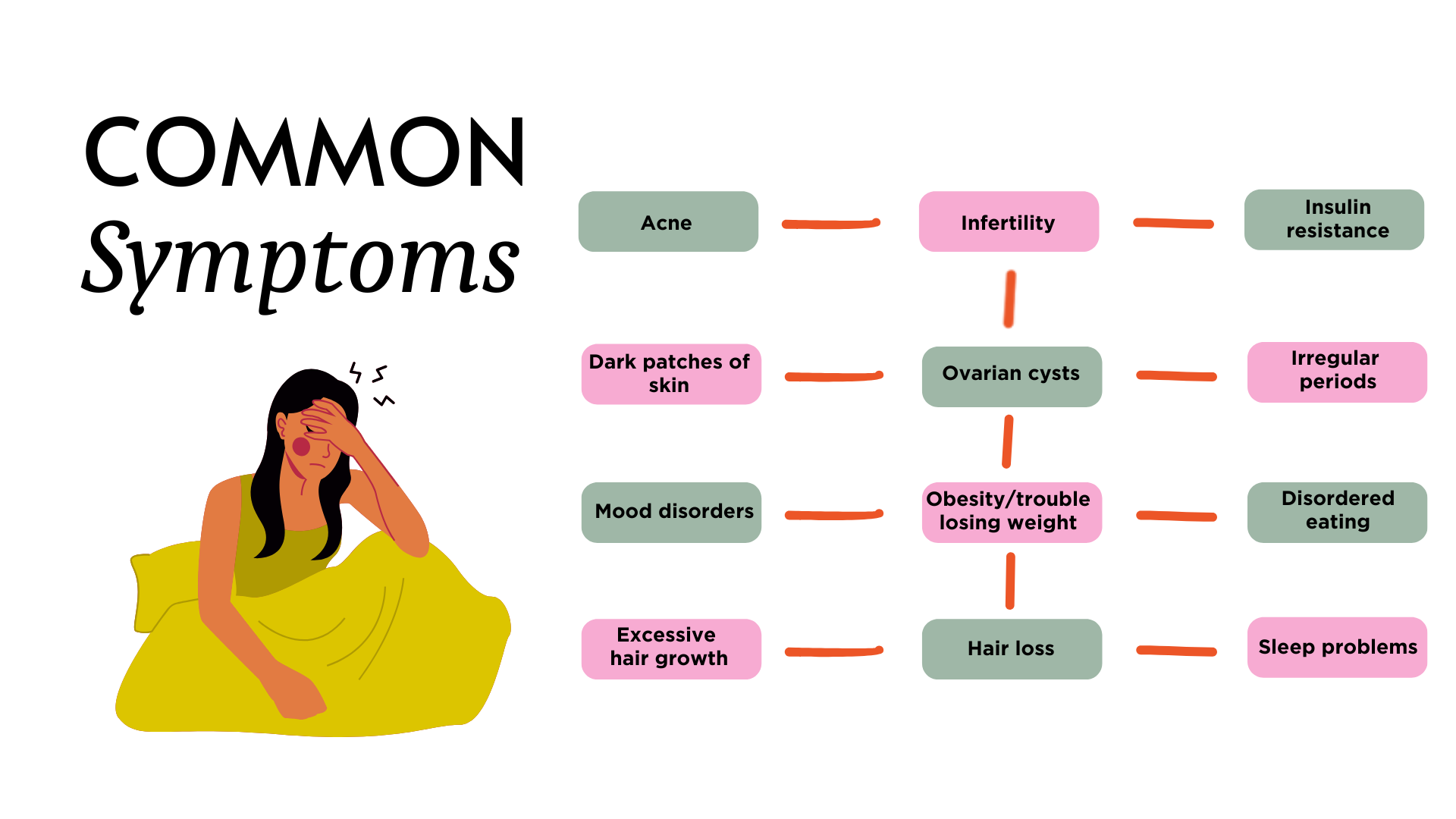
PCOS can present differently from person to person, but common symptoms include the following:
Individuals with PCOS are also at increased risk for other chronic health conditions, including type II diabetes, high blood pressure, high cholesterol, heart disease, endometrial cancer, sleep apnea, and chronic inflammation.
Mental health concerns—such as anxiety, depression, and other mood disorders—are also more common among individuals with PCOS.
Mental Health Prevalence and Risk
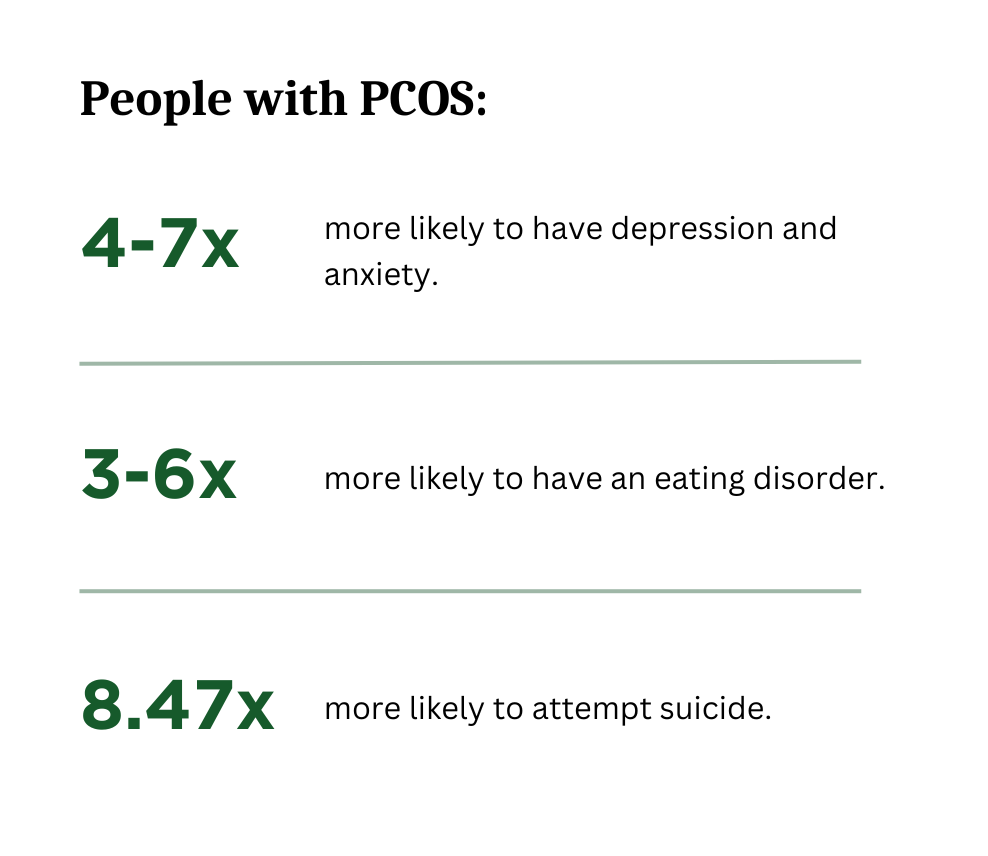
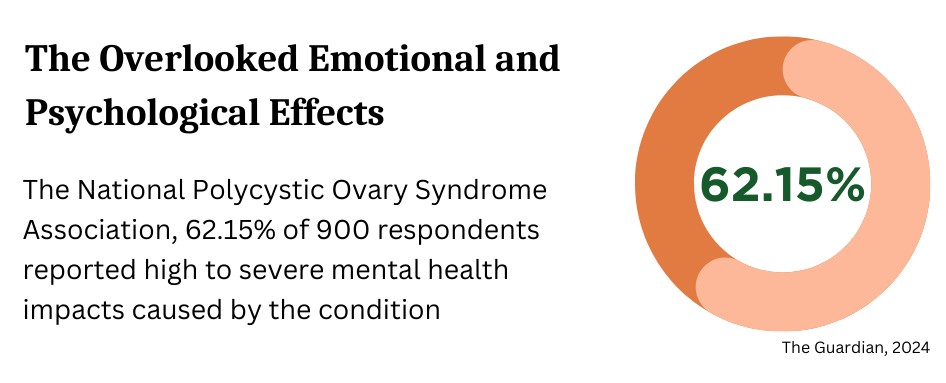
One of the most pressing concerns related to PCOS is its impact on mental health. Research has consistently shown elevated rates of psychological distress among people living with these conditions.
Recent studies have shown that people with PCOS are 4-7 times more likely to have depression and anxiety, 3-6x more likely to have an eating disorder, and 8.47x more likely to attempt suicide (The Guardian, 2024).
The exact cause of PCOS remains unknown, though evidence suggests a genetic component, as it often runs in families. Most treatment recommendations frequently focus on managing symptoms—such as birth control, dietary changes, weight loss, or managing any related health concerns—while the emotional and psychological impacts are often overlooked.
Why This Topic Matters to Me
My connection to PCOS is both personal and professional. I was diagnosed at twelve years old. I remember the doctor coming into the room, telling me I had PCOS, handing me a prescription for birth control pills, and telling me it would be impossible for me to get pregnant. There was no conversation surrounding follow-up, no discussion of long-term management, and no acknowledgement of how overwhelming that information might be for a child to hear. The message was simple: take these pills.
Over the years, I’ve heard strikingly similar stories from peers, friends, family members, and clients—many of whom were also diagnosed with PCOS or are still working towards a diagnosis. A common theme has been frustration and feelings of being dismissed. Many of them had to advocate repeatedly, or are still fighting to be taken seriously, in order to receive answers.
These patterns are part of what led me to focus my graduate capstone project on PCOS. The post is informed by my research and exploration of how PCOS affects mental health, identity, and emotional wellbeing—especially when some medical care can feel incomplete or invalidating.
Rose Paper Studio, 2023
A Note on Emotional Support
Living with PCOS often means managing more than physical symptoms. The emotional weight—uncertainty, grief, frustration, or feeling disconnected from your body—can quietly accumulate over time. Therapy can offer a space to slow down and make sense of these experiences, especially when they have been minimized or pushed aside. Rather than focusing on “fixing” something, counseling can support emotional processing, self-compassion, and coping in a way that honors the complexity of living with PCOS.
If you are looking for support with navigating the emotional impacts of PCOS, please reach out below.
References
Brady, C., Mousa, S. S., & Mousa, S. A. (2009). Polycystic ovary syndrome and its impact on women's quality of life: More than just an endocrine disorder. Drug, healthcare and patient safety, 1, 9–15. https://doi.org/10.2147/dhps.s4388
Daniella Bosman, Rose Paper Studio. (2023 and 2024). PNG.
Dybciak, P., Raczkiewicz, D., Humeniuk, E., Powrózek, T., Gujski, M., Małecka-Massalska, T., Wdowiak, A., & Bojar, I. (2023). Depression in Polycystic Ovary Syndrome: A Systematic Review and Meta-Analysis. Journal of clinical medicine, 12(20), 6446. https://doi.org/10.3390/jcm12206446
Francis, A. (2024, September 3). The invisible toll of life with polycystic ovary syndrome. The Guardian. https://www.theguardian.com/wellness/article/2024/sep/03/pcos-effects-mental-health
Gnawali, A., Patel, V., Cuello-Ramírez, A., Al Kaabi, A. S., Noor, A., Rashid, M. Y., Henin, S., & Mostafa, J. A. (2021). Why are Women With Polycystic Ovary Syndrome at Increased Risk of Depression? Exploring the Etiological Maze. Cureus, 13(2), e13489. https://doi.org/10.7759/cureus.13489
Polycystic ovary syndrome. (2023, June 28). World Health Organization. https://www.who.int/news-room/fact-sheets/detail/polycystic-ovary-syndrome